This week, we concluded the first phase of the TaSeRnet exchange program. Ten Radiation Therapy Technologists (RTTs) participated, exchanging knowledge across three proton therapy centers involved in the project. Over two days, RTTs observed clinical workflows and shared best practices focused on head and neck and esophageal cancer treatments.
Exchange Program Structure
Each morning, participants observed clinical activities such as CT simulation, image-guided proton therapy, and daily treatment. Afternoons were dedicated to discussions around best practices and workflow comparisons.
Key Discussion Topics
- Imaging Modalities: Centers using Cone Beam CT (CBCT) highlighted its advantage in soft tissue visualization, enabling more precise daily patient positioning. Others rely on 2D-kV imaging together with regular in-room CT scans. Matching protocols vary, with some centers using “traffic light” protocols to guide actions.
- Image Matching Expertise: Participants agreed that effective image matching requires both anatomical knowledge and an understanding of proton beam directions. Visualization tools such as 20% isodose lines were noted as helpful aids for deciding when discrepancies are clinically significant.
- Simulation & Immobilization: Simulation approaches differ between centers. Repositioning patients before the planning CT-scan to enhance reproducibility was seen as a best practice. Immobilization methods vary, especially for head and neck cases, including the use of masks, mouth spreaders, and specific positioning aids for arms and shoulders. While not universally applied, contrast-enhanced and dual-energy CT scans are recognized as valuable tools when available.
Importance of Training and Practical Insights
All teams emphasized the importance of well-trained RTTs and hands-on learning. Practical tips included using half CBCT scans to lower dose and providing personal towels for patient comfort.
Workflow and Role Variations
The exchange highlighted many similarities in proton therapy workflows but also revealed differences in RTT responsibilities across centers. These variations were the topic of meaningful discussions about protocol development and the influence of equipment and software on workflows and role distribution.
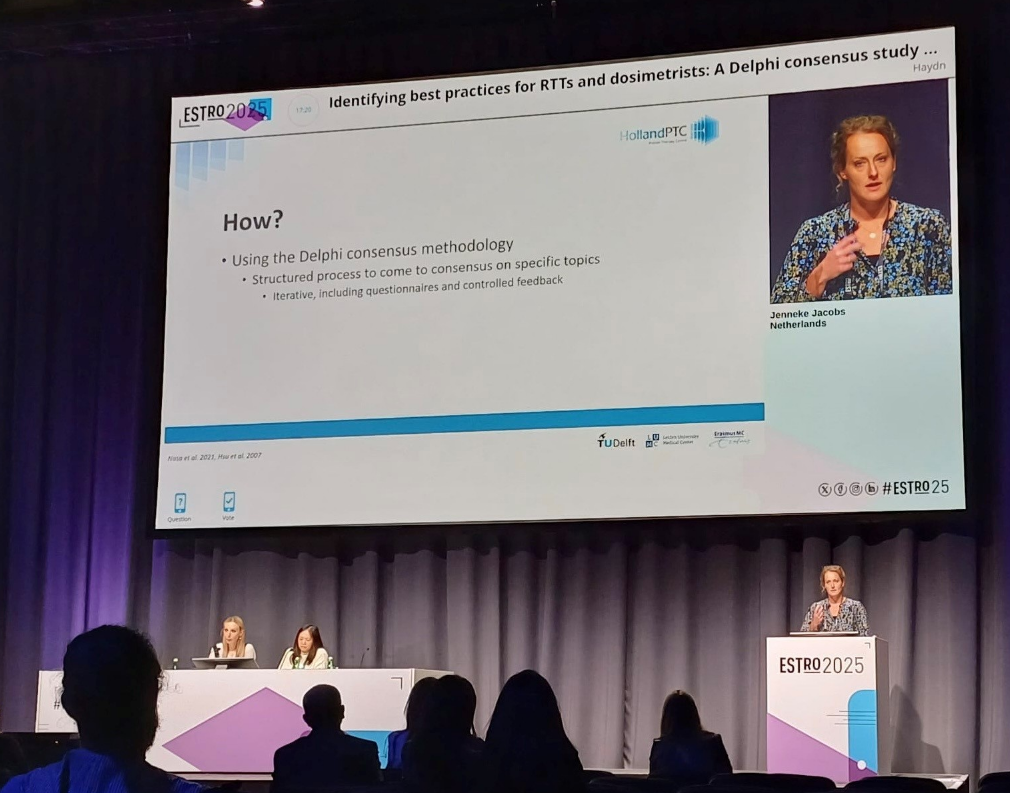
Reflections on Best Practice Implementation
At the end of the exchange, participants shared views on adopting best practices from other centers. While some had successfully implemented new approaches, most were open but faced practical barriers.
Facilitators for Adoption
- Implementation Plan: A clear and practical implementation plan was identified as the most critical factor for successful adoption. Participants stressed that clear communication about what is changing and how, is essential to avoid confusion and resistance. There was consensus that implementation plans and guidelines should be developed iteratively and support each other.
- Supporting Factors: Training and education, existing guidelines, and allocation of time and resources were also important. Although leadership support was ranked lower in a survey, discussion revealed it remains vital; management backing is crucial to secure the necessary time and staffing for implementation.
- Barriers: Participants identified time constraints, staff shortages, and multidisciplinary team approvals as the main hurdles to implement best practices. These challenges often stem from the practical reality of busy clinical environments.
Conclusion
The TaSeRnet job exchange has been a valuable opportunity for RTTs to reflect on current practices, share knowledge, and explore potential improvements. While enthusiasm for change is strong, successful implementation depends on structured planning, adequate support, and realistic resource allocation.